The Maternity Crisis in Australia is worsening:
why the silence?

One in three Australian mothers experience physical and emotional birth trauma. One in 10 emerges with post-traumatic stress disorder.
For many it begins with induction. From there women are at risk of the cascade of consent. First time mothers have over 40% chance of induced birth. Between 2000 and 2016 induction of labour tripled. Unnecessary inductions make up at least 15% of cases. This is of great concern.
The cascade of consent occurs when one intervention leads to another. An epidural may follow the induction. The epidural comes with a catheter and a drip. Labour slows, so synthetic oxytocin is given. From here, a caesarean or an assisted delivery becomes likely. Usually this cascade is not part of the consent process for the first intervention.
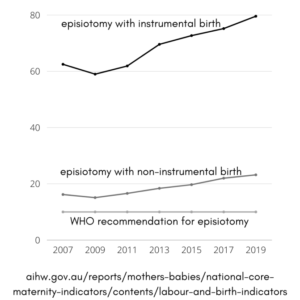
The purpose of consent is to ensure women are making informed decisions. Various exams and procedures require consent. This consent is usually in the moment, without deep discussion. This means women are consenting without realising that this is actually a decision point. A recent survey of Australian women found nearly 1 in 5 women may not have made an informed decision about the consent given for examinations or procedures they received during their maternity experience. The survey found 1 in 3 women who experienced birth with forceps or vacuum extraction, and 1 in 5 having a caesarean did not feel adequately informed. This is stressful for women, their partners and the care providers.
The consent approach to maternity care plays a big role in the latest statistics from the latest Mother and Babies Report. According to the report, the Australian maternity system processes women in 830 different policy driven approaches across 11 model categories. This lack of consistency impacts the decision making for women. Policy is presented as fixed, and consent is sought rather than a decision making process followed, ignoring women’s rights to choose alternative care pathways.
The data presented in the report is based on a select group of women:
“Selected women include those aged between 20 and 34 years, whose baby’s gestational age at birth was between 37 and 41 completed weeks, with a singleton baby in the vertex presentation. Comparison of ‘selected’ groups of women allows for an indication of standard practice. Selected women, for these indicators, refers to a cohort of mothers who are expected to have reduced labour complications and better birth outcomes. The proportion of selected women is approximately one-third (29.2%) of all women who gave birth in 2019.”
This is to say – they selected the group to give the best representation of the state of the Australian maternity system. The older Mothers report shows higher rates of intervention, suggesting this need lies with women, but is this really the case? These reports do not break down the data by model of care. It does, however, tell us that the bigger the hospital, the more interventions.
Women are the collateral damage in a system that refuses to provide adequate staffing and support for student midwives; we fail to ensure physiologically safe experiences for women and babies. Continuity of midwifery care reduces the risks of poor outcomes significantly. Less than 10% of women can access this model of care. The report excludes data from birth centres, which conveniently means we cannot compare the differences in this model of care. Meanwhile, the intervention rate continues to rise, and there is no action to implement the known solutions.
These failures of the system place women on a conveyor belt to be processed. This management approach deprives women of support during this significant life event. The COVID-19 pandemic has intensified this crisis, with reports of disrupted quality of care across many global settings.
What will the next Mother and Babies report show? The current report displays 2019 data, and shows the stark increases since 2004. These graphs collate the data, overlaying the rates in birth indicators showing how they have changed since 2007.
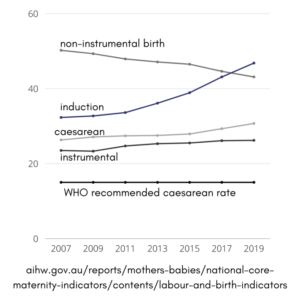
Of note is 2009. A dip indicates a reduction in intervention; followed by increases, particularly in induction.
In 2009, Nicola Roxon was the Health Minister. Kevin Rudd was Prime Minister, and in September women and midwives marched at The Mother of All Rallies at Parliament House in Canberra. It was a cold and rainy day and they turned up in the thousands!
For a brief moment, with the spotlight on the system, improvements were evident. And when the spotlight moved, interventions rapidly increased.
These increased interventions have not reduced mortality. With this increase in intervention we have seen an increase in birth trauma and PTSD related to the experiences. We are seeing midwifery burnout, under staffed maternity units are stretched and women are suffering the consequences.
For women to emerge into mothering more confidently they need effective communication and respectful maternity.
It is up to consumers to demand better service.
Join Maternal Health Matters to add your voice in support of consumer needs.
Our combined voices will forge change.
Author: Catherine Bell, MHM Board member and PhD candidate. Thank you Catherine.
